With the aging baby boomer population and the continued growth of the medical sector in Texas, the demand for healthcare services is expected to increase significantly over the next decade. The shift to electronic health records and the need to ensure that medical documentation is accurate for reimbursement continue to drive this demand. This translates to more opportunities for certified medical billing and coding jobs specialists in various healthcare settings.
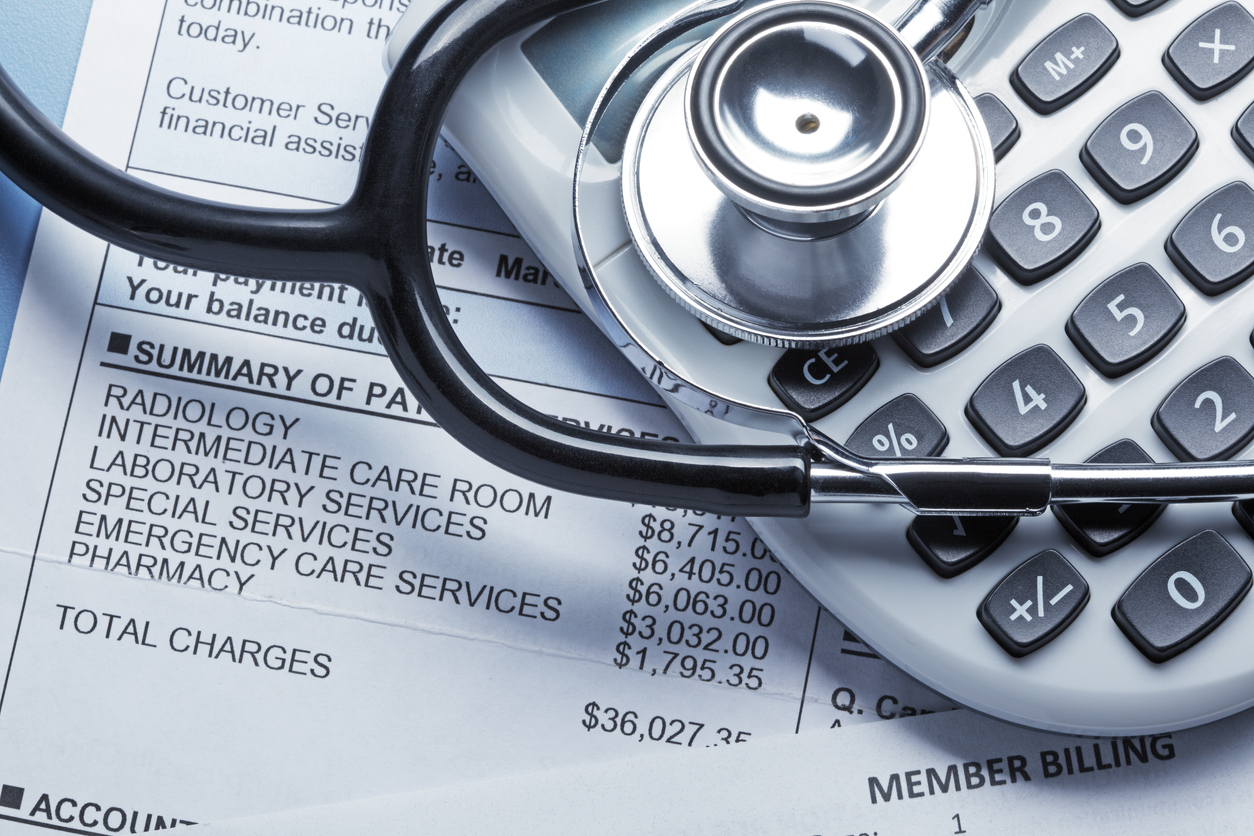
Medical billing and coding are essential processes in administering adequate healthcare services. They work to:
- Ensure healthcare providers receive accurate and timely reimbursement for their services
- Patients understand their medical bills and insurance claims
Medical coding involves translating medical diagnoses, treatments, and procedures into a universal language that treatment facilities and insurance providers share. The medical coder assigns specific codes to all services provided during a patient’s visit, including doctor consultations, laboratory tests, and imaging procedures. Healthcare providers and insurance companies use these codes to communicate patient care and payment.
On the other hand, medical billing is the process of submitting healthcare claims to insurance providers or government programs for recompense. The billing process starts with the healthcare provider documenting the services provided to a patient. Then, a medical biller uses the documentation to create a claim that includes the patient’s demographic and insurance information, the services provided, and all associated costs. Once the claim is submitted, the medical biller follows up with the insurance provider to ensure the payment is processed.
Medical billing and coding jobs have plenty of opportunities for growth and advancement. After completing the training program, graduates can work in various roles within the healthcare industry:
Medical Records and Health Information Technician
Medical records and health information technicians manage patients’ medical records to be accurate and up-to-date. These professionals use electronic health record systems to organize, code, and maintain medical records. They also safeguard medical records, ensuring they are kept confidential and secure. Medical records and health information technicians are hired in hospitals, private medical practices, and healthcare facilities.
Medical Billing and Coding Specialist
Medical billing and coding jobs specialists are an integral component of healthcare administration. Their role involves:
- Preparing and submitting claims to insurance companies and third-party payers for patient services.
- Analyzing and interpreting medical documentation and assigning appropriate medical codes to diagnoses, treatments, and procedures using a standardized coding system for accurate billing and reimbursement by insurance companies and other payers.
If you choose this career path, you will work closely with healthcare providers, insurance companies, and patients to ensure all billing and coding processes are accurate and efficient. You may also be responsible for verifying patient insurance coverage, obtaining pre-authorizations for medical services, and resolving billing and coding discrepancies.
Medical billing and coding jobs specialists must understand medical terminology, anatomy, and coding systems. Almost all healthcare settings need a medical billing and coding specialist.
Patient Access Representative
A patient access representative (PAR) serves as the first point of contact between patients and the healthcare system. They are in charge of the administrative aspects of patient care. When a patient walks into a facility, a PAR gathers preliminary information from them and verifies their insurance coverage and medical history. Their primary role is crucial in ensuring that patients receive the care they need in a timely and efficient manner.
Typically employed in multiple healthcare settings, PARs perform a range of duties that may include scheduling patient appointments, registering new patients, verifying insurance coverage and obtaining authorizations, collecting patient information, and processing payments. They also assist patients with questions about their healthcare options, provide information about medical procedures, and help clients navigate the healthcare system.
Every healthcare facility hires a patient access representative. Individuals who choose this career make a meaningful impact on patient care and are integral in improving the overall quality of healthcare services.

Medical Claims Processor
When you file a claim with your health insurance provider, it is the task of the medical claims processor to review and analyze your claims. They ensure your application is accurate, complete, and compliant with healthcare regulations and insurance policies.
Medical claims processors are responsible for verifying patient information, reviewing medical documentation, and processing claims for reimbursement. They also collaborate with healthcare providers to resolve any issues that may arise during the claims process.
To qualify as a medical claims processor, you must have strong analytical and decision-making skills and a deep understanding of insurance policies and medical billing procedures. They are employed in the insurance sector, with healthcare providers, or by government agencies that provide insurance coverage.
Medical Receptionist
A medical receptionist manages the front desk of a healthcare facility. They are responsible for answering phone calls, scheduling appointments, registering patients, and managing patient information. Medical receptionists may also be tasked with verifying insurance coverage, collecting co-payments, and assisting with billing and coding procedures. Their primary focus is on providing excellent customer service to patients, ensuring they have a positive experience when visiting the facility.
Requirements to Work in Medical Billing and Coding in Texas
To work in a medical billing and coding job in Texas, one must complete a postsecondary training program in medical billing and coding. The certificate course typically takes about one year to complete and can be taken online.
Certification can be provided by professional organizations such as the American Academy of Professional Coders (AAPC) or the American Health Information Management Association (AHIMA). Some employers require applicants to provide proof of training. So having credible certification comes in handy in such situations.
All medical billing and coding jobs are classified under health information technician in the state of Texas. Professionals under this group can work anywhere without a license. What this means is you can apply for a job as soon as you’re done with your training.
Students interested in the medical billing and coding field need to research job requirements before making applications. Then seek guidance from your school’s career center or program advisor to ensure you’re on track to meet the necessary qualifications.
Get Started Today
The outlook for medical billing and coding careers in Texas is optimistic, driven by an aging population requiring more medical services and an increasing demand for electronic health records. Interested in medical billing and coding careers? SCI can help train you on the skills needed to pursue a medical billing and coding career through our online program.
Southern Careers Institute focuses on equipping interested individuals with the most appropriate skills that can increase their chances of getting employed. Contact us today to seek more information about the online Medical Billing and Coding Specialist program at SCI.
This article was published on: 03/20/23 4:16 PM
* SCI does not guarantee employment or a starting salary upon graduation, completion, or withdrawal from SCI. As an accredited post-secondary institution, SCI has various federal financial assistance programs available for students who qualify and are enrolled in SCI programs. This does not apply to seminar students.
GI Bill® is a registered trademark of the U.S. Department of Veterans Affairs (VA). More information about education benefits offered by VA is available at the official U.S. government Web site at http://www.benefits.va.gov/gibill.